Transcranial Magnetic Stimulation
Smart. Focused. Drug-free.
TMS therapy uses a highly focused, pulsed magnetic field to stimulate under-active brain regions believed to be involved with depression. The magnetic pulses are similar in type and strength to those produced by a magnetic resonance imaging (MRI) machine.
Transcranial Magnetic Stimulation (TMS therapy) is effective, and FDA approved for depression and is a particularly good choice for patients who have not fully responded to antidepressant medication, or for those who experience side effects with antidepressant medication.
TMS therapy is performed in the privacy of our office. Patients remain awake and can go right back to their usual activities after a treatment.
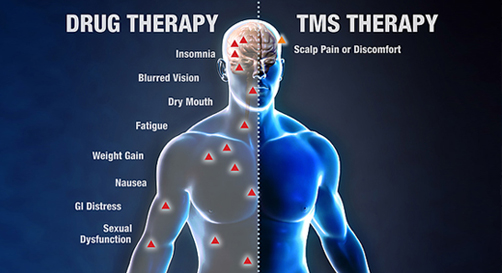
Typical TMS side effects are transient and include mild discomfort at the treatment site and headache. TMS therapy does not cause weight gain or sexual dysfunction, which are common longer-term side effects with antidepressant medication.
In clinical trials, less than 5% of patients discontinued TMS treatment due to side effects.
Neuroimaging studies show that TMS therapy results in improvements in metabolism in the brain areas involved in mood and normalization of the circuit. Further, TMS stimulates nerve growth factors and sprouting of nerve cells, as seen with other successful antidepressant treatments. TMS is also being studied in many other brain disorders, including anxiety disorders, Parkinson’s disease, and Alzheimer’s disease.
Brain Networks

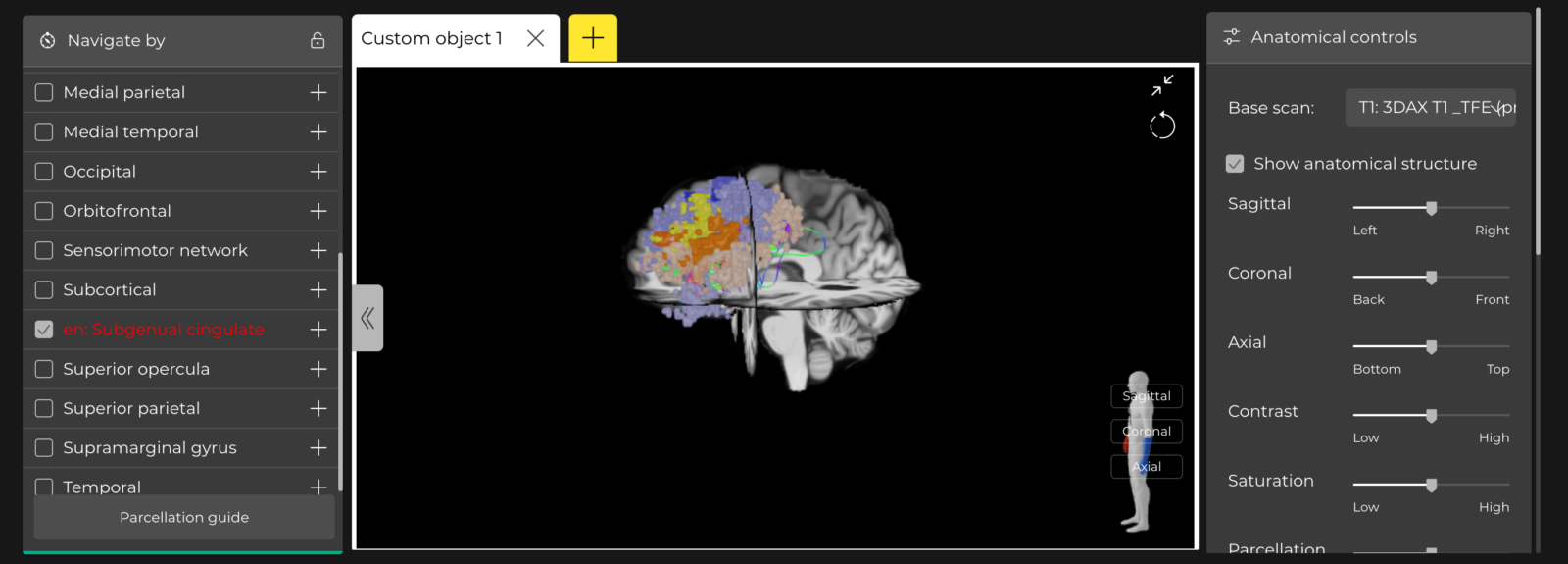
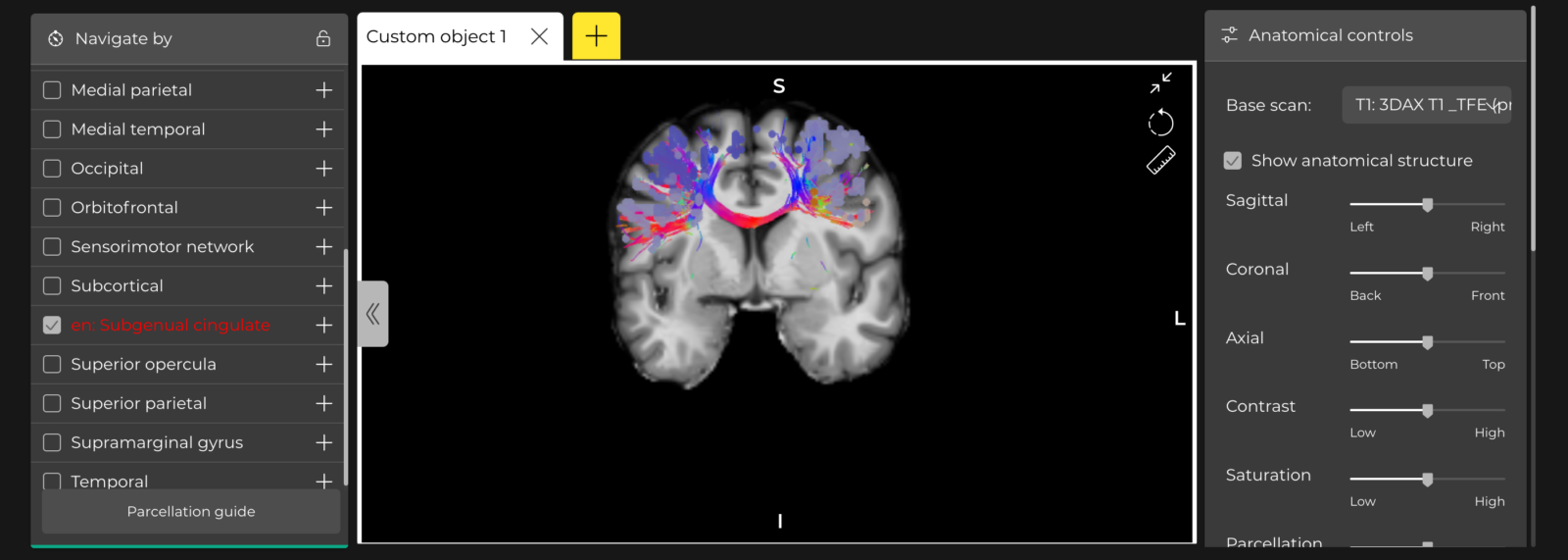
Brain networks: collections of parcels that are connected by tracts and activate together to perform a specialised function.
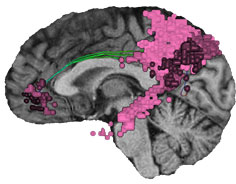
Default mode network (DMN)
Salience (SN)
Central executive network (CEN)
Yeo, B.T., Krienen, F.M., Sepulcre, J., Sabuncu, M.R., Lashkari, D., Hollinshead, M., Roffman, J.L., Smoller, J.W., Zöllei, L., Polimeni, J.R. and Fischl, B., 2011. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. Journal of neurophysiology.
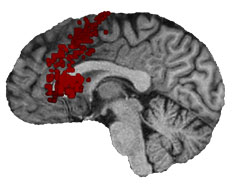
rTMS version 1 is imprecise. Targets in version 1 are based on measurements on the skull (5 cm rule, F3, helmets or even EEG.


We use MRI and functional networks for precise individual targeting, as used in SAINT or Stanford Neuromodulation.
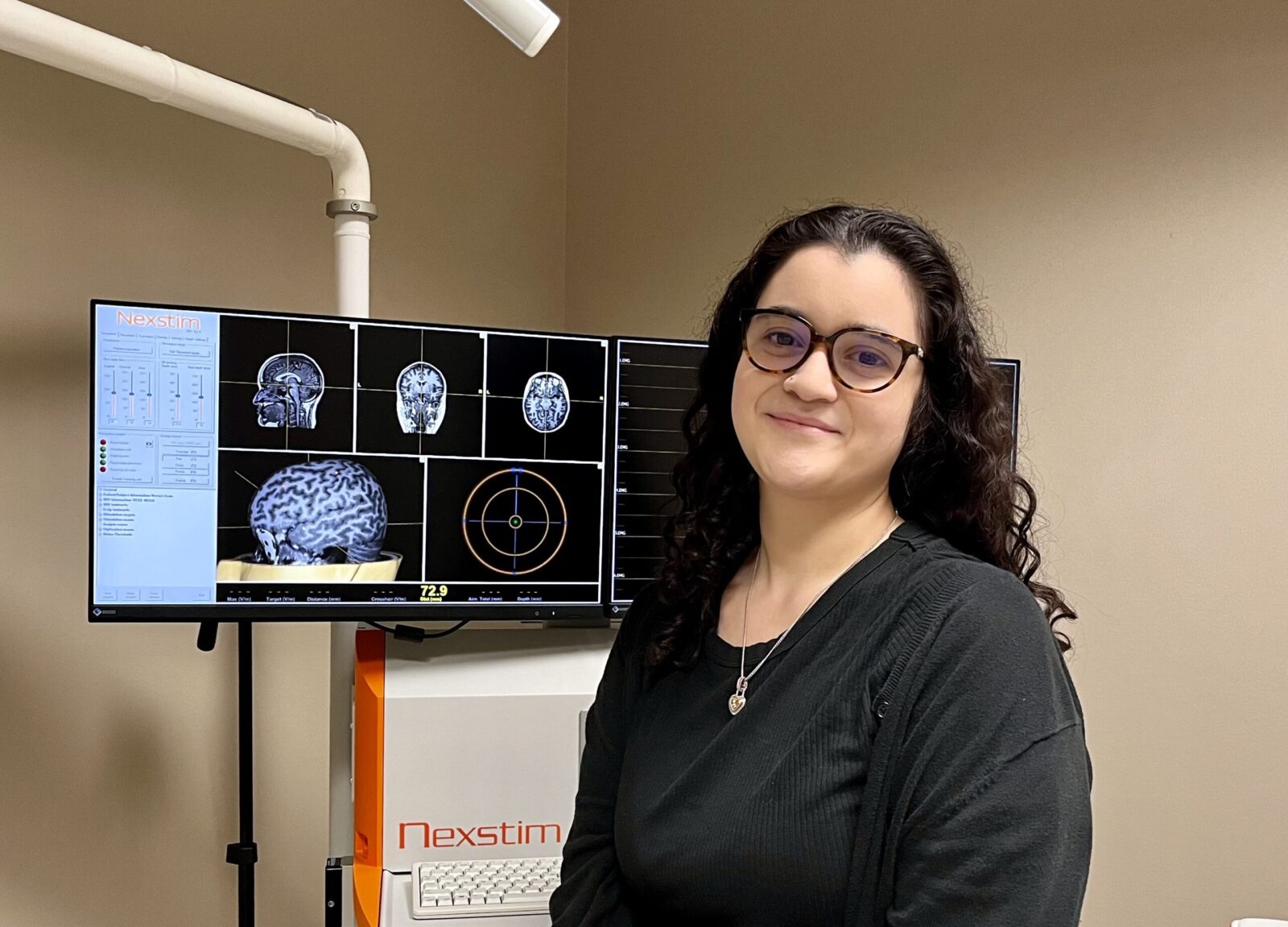
What’s NEW? NEURONAVIGATION:
A Better TMS Solution Based on Science.
Anyone administering TMS needs the tools to make sure the right dose of TMS therapy is given to the right part of the brain. Other TMS systems deliver the magnetic pulse to a location that is estimated based on skull measurements or placement of a helmet on your head. We use an MRI scan of your own brain, as you would in neurosurgery.
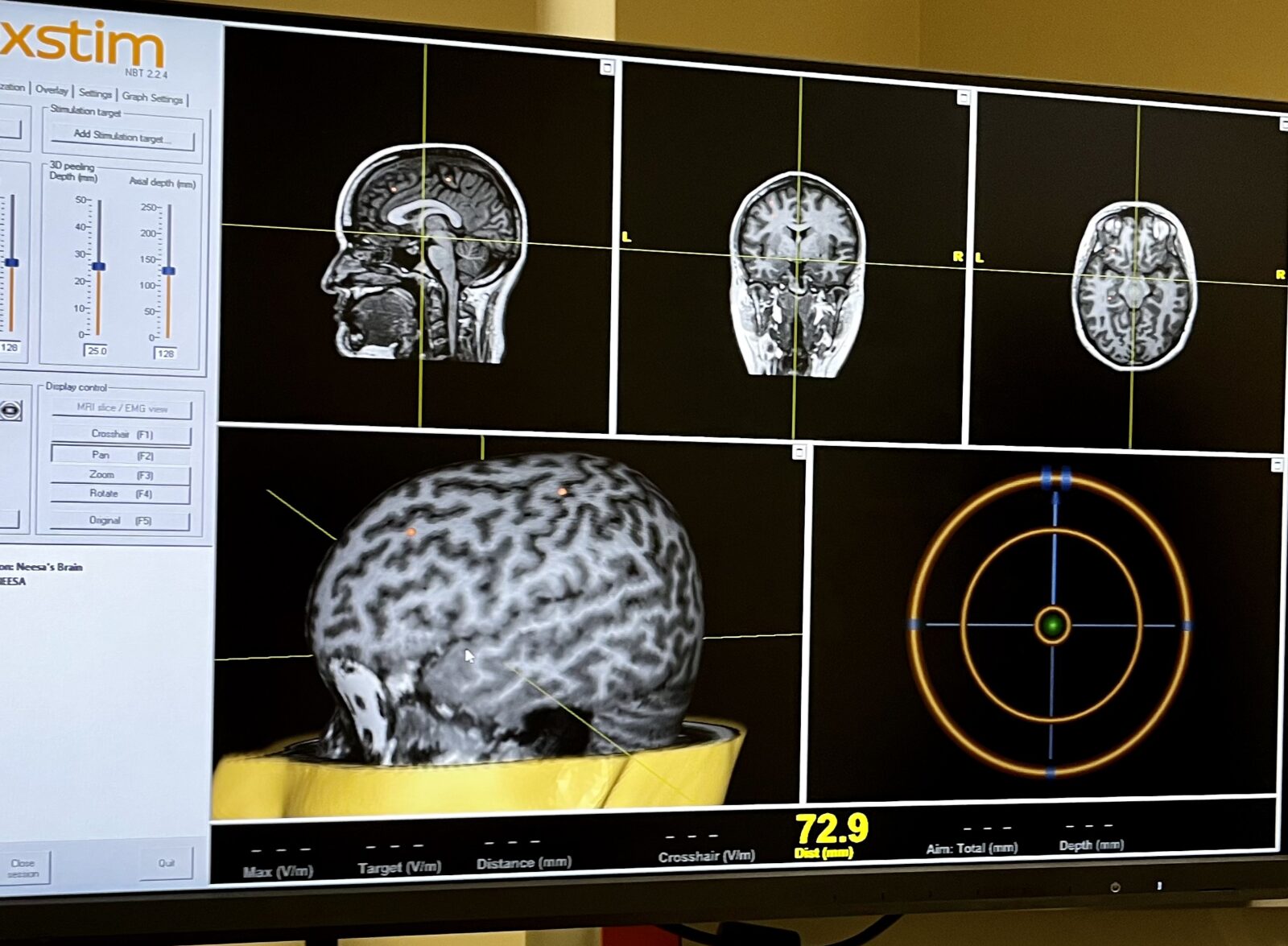
scan using nexstim technology
call us at (713) 489-5000!
Transcranial Magnetic Stimulation
Smart. Focused. Drug-free.
TMS therapy uses a highly focused, pulsed magnetic field to stimulate under-active brain regions believed to be involved with depression. The magnetic pulses are similar in type and strength to those produced by a magnetic resonance imaging (MRI) machine. Transcranial Magnetic Stimulation (TMS therapy) is effective, and FDA approved for depression and is a particularly good choice for patients who have not fully responded to antidepressant medication, or for those who experience side effects with antidepressant medication. Typical TMS side effects are transient and include mild discomfort at the treatment site and headache. TMS therapy does not cause weight gain or sexual dysfunction, which are common longer-term side effects with antidepressant medication.
TMS therapy is performed in the privacy of our office. Patients remain awake and can go right back to their usual activities after a treatment. In clinical trials, less than 5% of patients discontinued TMS treatment due to side effects.
Neuroimaging studies show that TMS therapy results in improvements in metabolism in the brain areas involved in mood and normalization of the circuit. Further, TMS stimulates nerve growth factors and sprouting of nerve cells, as seen with other successful antidepressant treatments. TMS is also being studied in many other brain disorders, including anxiety disorders, Parkinson’s disease, and Alzheimer’s disease.
TMS for depression, using the standard dosing protocol of five times a week for 6 weeks, is covered by many insurance plans, typically with preauthorization.
What’s NEW? NEURONAVIGATION:
A Better TMS Solution Based on Science.
Anyone administering TMS needs the tools to make sure the right dose of TMS therapy is given to the right part of the brain. Other TMS systems deliver the magnetic pulse to a location that is estimated based on skull measurements or placement of a helmet on your head. We use an MRI scan of your own brain, as you would in neurosurgery.
As a matter of fact, we use a TMS machine that was developed for neurosurgery with sophisticated software to model the complexity of your individual head (Nexstim.com). This is called neuronavigation or nTMS. If you can’t see your actual brain when you are getting TMS, your doctors are not getting the information to know the best location to stimulate. The use of neuronavigation is FDA approved for neurosurgery, neurology, and psychiatry.
Introducing Accelerated TMS
We can do more than one treatment in a day to consolidate the treatment course. For example, 36 treatments, or more, can be administered in as short as a week. Many of our patients choose to break the session up over two weeks. Accelerated TMS. Multiple studies have shown that getting better from depression with TMS is related to the number of treatments, not the number of days or weeks.
As a matter of fact, we use a TMS machine that was developed for neurosurgery with sophisticated software to model the complexity of your individual head (Nexstim.com). This is called neuronavigation or nTMS. If you can’t see your actual brain when you are getting TMS, your doctors are not getting the information to know the best location to stimulate. The use of neuronavigation is FDA approved for neurosurgery, neurology, and psychiatry.
EVEN BETTER: FUNCTIONAL NETWORKS
Individual brain areas activate to perform specialized functions such as seeing, hearing or thinking. This is called a network. Networks important in psychiatry include the Default Mode Network (DMN), the Salience Network and connections to the dorsal lateral prefrontal cortex (DLPFC) and the subgenual cingulate areas of the brain. Normal brain function relies on brain networks communicating properly with each other and themselves. Using functional MRI and sophisticated software (Omniscient, Sidney Australia), we are now able to overlay these key networks, based on your fMRI. We combine our decades of clinical experience with all available data to provide unparalleled personalized TMS targeting for you.
Frequently Asked Questions
Is Nexstim TMS the same as “Deep” TMS?
No. Nexstim can deliver a pulse that effectively reaches at least 3-4 cm below the scalp. And since the cortex is directly and indirectly connected to deeper areas of the brain, stimulation of specific cortical locations, as determined by the persons own MRI scan, can normalize abnormal circuits deep within the brain. The circuit location is even more precise when functional MRI (fMRI) is superimposed on structural MRI. What is often called “deep” TMS, typically delivered by a helmet, is less specific.
Are these networks like the SAINT, or Stanford Neuromodulation Therapy (SNT)?
‘SAINT’, or SNT targets the spot where the left dorsolateral prefrontal cortex (DLPFC) is most closely connected to the subgenual anterior cingulate cortex (sgACC). In patients with depression, the DLPFC is underactive and the sgACC is overactive. The hypothesis is that DLPFC controls the sgACC, so stimulating the specific area in the DLPFC that has the best network connection to sgACC will normalize the network. We look at this relationship as well as relationships in other areas of the DMN and SN.